Today's pacemakers are truly remarkable devices. Most of them can be programmed in literally millions of possible combinations. Their main purpose is to keep the electrical system from going too slow and thereby prevent the problems associated with slow heart rhythms (passing out, congestive heart failure, and others including death). Pacemakers are necessary because, while there are many medications that prevent tthe heart from going too fast, there are only a handful that make it go faster. Those that speed the heart rate are poorly tolerated and very often associated with serious side effects. Pacemakers have become a reliable means of helping people live longer and improve their lifestyles despite having a slow heart rhythm. Newer types of pacemakers can correct some types of rapid heart rhythms as well.
Below are most of the most common questions about pacemakers. If you have more or different questions, be sure to check out the other areas about arrhythmias on HeartPoint. They are listed at the bottom of this page.
GENERAL
Why do I need a pacemaker?
What kind of pacemakers are there?
What does a pacemaker look like?
IMPLANTING PACEMAKERS
How are pacemakers put in?
Will it hurt?
Will people be able to see that I have a pacemaker?
Can anything go wrong when a pacemaker is placed?
How do leads stay in place?
What happens after the pacemaker is placed? How do I make sure everything stays in place?
Is there anything I should watch for?
AFTER THE PACEMAKER IS IMPLANTED
Do I need to do anything after I get my pacemaker?
What things about the pacemaker can be "programmed"? How is it done?
What happens when I check out my pacemaker on the phone?
What do I need to do to keep my pacemaker working properly?
How long do they last?
My pacemaker is designed to beat faster when I do more. How and why is that done?
CONCERNS AND PROBLEMS
What happens when the battery runs out?
I've heard I need to be careful around microwave ovens. Is this true?
Are there things that can reprogram my pacemaker accidentally?
How do I know my pacemaker is still working?
I feel my shoulder twitch when my pacemaker goes off. Is this normal?
My pacemaker is "set" for 70. Sometimes I take my pulse and it's only 64. Is it broken?
GENERAL
As you might suspect, there will not a simple answer to this one -- patients require pacemakers for many different reasons. Most pacemakers are placed to prevent the heart from going too slow. Most often, this occurs because there is no cell in the heart that will beat fast enough to maintain proper function, or because there is a "block" somewhere in the electrical pathway which doesn't allow the electrical activity to spread to all of the necessary portions of the heart muscle. The underlying cause of this may be scar tissue, most frequently from previous heart attacks. Sometimes it is simply caused by "aging" of the conduction system.
The devices used for rapid heart rhythms may provide a reliable means of converting dangerously rapid rhythms (such as ventricular tachycardia or ventricular fibrillation), or an alternative to medications for patients with occasional bouts of atrial fibrillation.
What kind of pacemakers are there?
Several kinds are used. Most of the devices implanted today are for correcting rhythms that are too slow, and are discussed below. Devices for rapid rates ("AICD's" or defibrillators) will be covered in another area of HeartPoint soon. Pacemaker leads may be placed in the atrium alone, the ventricle alone, or in both the atrium and ventricle depending on the situation.
Single lead pacemakers are used primarily in four situations:
1. When the only problem is with the formation of the initial impulse in the atrium, simply placing a lead in the right atrium will "start things off" when it's needed, and the electrical impulse will then continue normally through the rest of the atrium, the AV node and the ventricles.
2. When the patient is in chronic atrial fibrillation and the ventricle is going too slow atrial fibrillation. In this case, only a single lead is placed in the ventricle (because the fibrillating atrium cannot be paced).
3. When the problem with a slow rate occurs only occasionally and for relatively brief periods of time, a single lead in the ventricle may be all that is utilized to provide brief help at those times.
4. A special lead which can sense in both chambers, and pace only in the ventricle is also useful in some situations, and is discussed below.
"Dual chamber" devices (with one lead in the right atrium and one in the right ventricle) are desirable in many situations. Such devices keep the upper and lower chambers contracting in their proper sequence.
A fairly recent development is a single lead that paces only the ventricle, but senses both chambers. In this device, a sensing ring is on the lead at the level of the atrium, which can sense the atrium's activity. The ventricle is sensed in the usual way, via the contact of the lead with the muscle. This device is particularly useful in situations where the sinus node is beating fast enough, but there is a block in the propagation of the impulse to the rest of the heart muscle.
The earliest pacemakers did not sense if the heart was making any impulses on their own, and were described as "fixed rate" pacemakers. These are simply not made any longer, and current devices are described as "demand" models, pacing the heart only when needed.
Another feature that distinguishes different types of pacemakers is their ability to respond to a person's activity, going faster when the person is active, and slower when inactive.
Most modern pacemakers can be programmed, and can be set in a manner that is best for the particular person in whom it is implanted. There is more on this below.
What does a pacemaker look like?
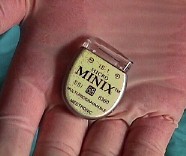
A pulse generator, which contains both the battery and the intelligent circuits, can be very small, as seen here. This device can be connected to a lead which makes contact with either the atrium or the ventricular muscle.
Shown here are two leads. The one on the top is a lead with a "J"
shape, which is used for optimal positioning in the atrium. It is "unipolar",
and therefore smaller, and is a "tined" lead which makes passive contact with
the atrial muscle.
In contrast, the lead on the bottom is larger because it is a bipolar device which has more wire within it. It has a small screw at the end so that it can be actively fixated to the muscle.
Both leads are shown at higher magnifications below.
Here, a pulse generator is shown which is connected to two leads, for dual-chamber pacing. Despite it's sophistication, it is still quite a small device.
The two major types of leads are shown here. On the left is a magnified view of a screw-in lead. The lead on the right is a "tined" lead, which uses the small plastic tines to become passively "stuck" to the muscle in either the atrium or ventricle.
In either case, the leads will grow firmly attached to the heart muscle, and will be difficult to remove after 6 months.
How are pacemakers put in?
Generally, the insertion or "implantation" of a pacemaker is considered minor surgery. In most cases, only sedation (and not general anesthesia) is utilized. Local anesthetic is used to numb the area over where the pulse generator will be placed. An incision is made and a "pocket" is formed in the area overlying the muscle on the outside of the chest wall. The pocket needs to be big enough to house the pulse generator, most of which nowadays are about 3 inches by 2 inches in size, and are less than one-half of an inch in thickness. Shown below are two different pacemakers.
The pacemaker leads are made of a wire covered by a flexible insulating substance. These are introduced into a vein near the site of the pocket, and then advanced through the large veins that lead to the heart. An x-ray tube ("fluoroscope") is used to visualize the leads and heart structures so that the leads can be placed in a satisfactory position. They are then "tested" to see how well the underlying electrical activity of the heart is sensed ("sensing threshold"), and how little energy is required to capture the muscle ("pacing threshold").
The leads are inserted into the pulse generator, and tightened down with a specialized screwdriver. The pulse generator is then usually secured to the underlying muscle with a suture. The wound is closed using a variety of techniques. This generally requires about 30-60 minutes to complete, although sometimes there are technical challenges which cause the procedure to last quite a bit longer.
Will it hurt?
It can. Sedation is used to minimize this, as are local anesthetic agents. There are certain parts of the procedure which can be uncomfortable, although this is generally not severe. The surgical site will usually be uncomfortable for around one or two weeks. Analgesics such as aspirin, acetaminophen, or ibuprofen can be used. Some people do have discomfort which stays with them as long as the pacemaker is in. This is unusual however, and is generally mild and treatable with analgesics.
Will people be able to see that I have a pacemaker?
There will be a scar about 2-4 inches long.
The pulse generator as previously noted is about 3 x 2 by less than one-half inch thick. On some people, especially those who are quite skinny, it can be noticeable. On heavier people, this may hardly be noticeable at all.
Can anything go wrong when a pacemaker is placed?
- Certainly, but they are generally uncommon.
- Infections can always occur, and may require antibiotics or further surgery.
- Bleeding likewise will occur to some degree with any surgery, but is generally minimal with this procedure. However, there is always some chance of severe bleeding which may require transfusion.
- The technique often includes gaining access to a vein using a needle advanced under the collar-bone. If this technique is used, the needle may puncture a lung, and cause the lung to collapse. A tube may need to be placed in the chest cavity for several days until this puncture seals itself off. It is conceivable that the chest will have to be surgically explored to seal the puncture in some cases (possible, but very, very unlikely).
- Sometimes the pacemaker cannot be placed in one or both sides of the chest for a variety of reasons.
- Death as a result of pacemaker implantation is possible, but very, very uncommon.
How do the leads stay in place?
Some leads are termed "active fixation" (see pictures at the beginning of this section). These have some means of being secured to the heart muscle, typically a screw device. These decrease the tendency of the lead to move early after it is placed, but are often not as efficient in sensing and pacing in the long run.
The other main variety of lead is a "passive fixation" device (see pictures at the beginning of this section). These have little extensions off from the lead which become lodged in the irregular contour of the heart muscle. These have the advantage of often providing better long term performance in sensing the electrical impulses. However, they have a slightly greater incidence of becoming dislodged early after their placement.
In either case, the leads will become firmly attached to the heart muscle over time. Early after implantation, the leads will induce a mild inflammatory reaction. During this period of time, it will take more than usual amounts of energy to capture the muscle. Generally, the leads become very fixed to the muscle after about six months, and are difficult if not impossible to remove.
What happens after the pacemaker is placed? How do I make sure everything stays in place?
You should receive specific instructions on these matters before going home. Activities are generally limited to some extent because in the period after they are placed, the leads may move or be dislodged by overly vigorous activities. Often, just after the pacemaker is placed, a sling or "immobilizer" will be placed so that the arm is not moved too much, and this reminder will be kept in place for several hours to as long as a day or two. In general, you will be told not to overdo activities using the affected arm and hand for a period of time, generally one to two weeks.
Is there anything I should watch for?
Infection is always a threat after any surgery, but is unusual. This is an important consideration in a pacemaker because the device is a "foreign body", and it may be very difficult to treat an infection if it occurs. If you notice any of the classic signs of infection: redness, heat, or oozing of material (particularly if it is discolored), you should contact your physician or surgeon.
If you notice undue shortness of breath, this may indicate a problem with perforation of a lung. Although this is unusual, and if it does occur generally causes problems shortly after surgery, it may also occur within the first several days.
If your symptoms were initially cleared with the placement of the pacer and then return, this may indicate a malfunction of some sort, and you should contact your physician.
If you have undue pain at the pacer site, you should have it checked out.
Swelling of the arm and/or hand where the pacemaker was placed may indicate that a clot has formed in that vein, and requires prompt evaluation.
AFTER THE PACEMAKER IS IMPLANTED
Do I need to do anything after I get my pacemaker?
There are several things to remember:
- make sure you understand how to take care of the surgical wound. This will vary according to the surgeon who does the procedure and his particular techniques and preferences.
- You will need to have a recheck of the surgical wound at some point.
- In addition, your surgeon or someone he delegates will need to interrogate and often reprogram the device in 4-8 weeks after it's placed. This is to make sure everything is working properly. Furthermore, by this time the lead has "grown in" and the requirements for energy to capture the muscle have decreased. The pacer can then be reprogrammed to use less energy, and significantly prolong the life of the battery.
- You, or somebody at the hospital, will need to send in your pacemaker registration. You, and this information is tracked very carefully by the manufacturers. You will want to have your own record in case of any questions, particularly in an emergency.
- Make sure you have a copy of your pacemaker card. This should be sent to you within several weeks of the implant. If not, contact your physician.
What things about the pacemaker can be "programmed"? How is it done?
Pacemakers are indeed very advanced devices. One of their most desireable features is the ability to "program" them to behave in different manners according to the needs of the patient. This allows for the function of the device to be individualized for you. No surgery is necessary to do this - it is done through the skin, and indeed even through your clothes. The programmer "talks" to the pulse generator using radio frequencies. A typical device being used is illustrated below.
The most easily understood aspect or "parameter" that can be changed is the "lower rate" of the pacemaker: that is, the rate at which the pacemaker will "kick in" to prevent the heart from going slower than this rate. This is usually set at 50, 60 or 70 beats per minute.
Many other aspects can be programmed, including the strength and duration of the impulse delivered to the muscle, how fast the pacemaker will go, and the pause between stimulating the atrium and the ventricle. This is just the start of the possibilities.
What happens when I check out my pacemaker on the phone?
To save a lot of running around and traveling, yet to be able to make sure the device is working properly, pacers have been designed so that they can give out certain information without the need of being near a programmer. This "transtelephonic follow-up" is designed into every pacemaker. When the telephone device is placed over the pacemaker, it sends out sounds that can be carried over telephone wires. When "unscrambled" on the other end, an electrocardiographic tracing appears. To make sure the pacemaker is capable of pacing even when the patient's own rate is high, a magnet is present which makes the pacer send electrical impulses regardless of the patient's underlying rate.
The "magnet rate" contains information about the status of the pulse generator's battery. Each manufacturer programs this in a different but characteristic way. A certain "magnet rate" indicates the need for elective or immediate replacement for each model.
Keeping up with your telephone follow-up is very worthwhile!
What do I need to do to keep my pacemaker working properly?
Just keep up with the "scheduled maintenance"! There is really not much to this. Keep up with your scheduled "checks" over the telephone. In some instances, your physician may wish for your pacemaker to be interrogated and possibly reprogrammed on a yearly basis. The rest of it simply takes care of itself. Be sure to carry your pacemaker card with you.
How long do they last?
Pulse generator batteries generally last from 6-10 years. As they would say in the car business though, "actual mileage may vary". It depends on such factors as
- How often a given patient uses the pacemaker. That is, is the pacemaker simply sensing the heart's activity most of the time, or does it need to expend the energy to capture one or both chambers frequently or all of the time.
- How well it is programmed. Proper programming will minimize the use of energy.
- How good is the connection or "electrical interface" between the lead and the muscle. The best connections require the least energy.
- What medications the patient is on, since this may play an important role in how often the pacemaker is required to fire, and how much energy it must use.
- Whether there are any fractures of any of the leads. A fracture of the insulation or wire can lead to a rapid drain on the battery.
- The type and manufacturer of the device.
My pacemaker is designed to beat faster when I do more. How and why is that done?
One of the great advances in pacemakers was the ability to sense the patient's movement and have the pacemaker fire at a faster rate. This of course mimics what the person's own heart would like to do when activity takes place. People very simply felt better when their rate was not "fixed", but could vary.
The original type of sensor of activity was one that simply sensed movement. This device continues to be used, and is very satisfactory for many, many patients. The amount and duration of movement required to change the underlying rate can be programmed.
Despite this, the device can't tell whether you're going upstairs or downstairs . . . or scratching your head for that matter . . . it can just tell that you're moving. To overcome this type of problem, other types of sensors have been developed. Some will measure the temperature of the blood (which will rise with increasing activity), others utilize estimates of the size of the heart chamber, others various intervals on the electrocardiogram, etc. Some of these more sophisticated methods require special leads - and corresponding compatibility problems. One of the most recent devices adjusts its rate to vary according to how hard the person is breathing, and does so with standard leads.
PROBLEMS AND CONCERNS
What happens when the battery runs out?
Pacemaker batteries are designed to become depleted in a slow and predictable fashion. When followed over the telephone, the steady decline in energy can be followed. When the battery is low but still has significant power left, the pacemaker will still work just fine, but give indications (peculiar to each manufacturer and model) that the time for replacement is nearing. When the ERI (elective replacement interval) is reached, plans can be made for changing the battery at a date convenient for the patient and the surgeon.
Even beyond the ERI, pacemakers continue to pace for a long time, and do not simply stop emitting electrical energy suddenly or unexpectedly.
When it's time for a new pulse generator, it is generally simply exchanged for a new one. This will require surgery to remove the old device. The leads will be unscrewed and removed from the old generator, and then tested to make sure they are still working well. If not, new leads are placed. Most of the time however, they are still found to be working well and are simply attached to the new generator and placed back in the pocket, which is closed as it was before.
The new generator is almost always much smaller than the one it replaced due to advances in the design and manufacture of pacemakers.
I've heard I need to be careful around microwave ovens. Is this true?
Not unless your unit is very, very old. Microwaves were used in the "old" days to communicate with the pulse generator so it could be interrogated and reprogrammed. It was therefore subject to interference from other devices which produced microwaves, such as ovens. Even then, they had to be really leaky.
Nowadays, I warn my patients that as long as they don't get in a microwave and turn it on, that they should be safe.
Are there things that can reprogram my pacemaker accidentally?
Yes. Arc-welding can create a high energy field that will reprogram pacemakers. In addition, cellular telephones, particularly the digital variety can cause problems. For more about the problem with telephones, follow the link to Pacemakers and Cellular Phones.
How do I know my pacemaker is still working?
You have to get it checked, either over the phone or in person.
I feel my shoulder twitch when my pacemaker goes off. Is this normal?
This usually is not normal, but it may not be a major problem. This is caused from stimulation of muscles of the chest wall, particularly those right under the pulse generator. It is more common in "unipolar" devices, which use the entire body as part of the grounding lead, than it is in "bipolar" devices whose circuit is much smaller, typically involving only the tip of the lead.
Usually, programming can minimize or completely solve this problem.
My pacemaker is "set" for 70. Sometimes I take my pulse and it's only 64. Is it broken?
This is a very common question, and is fueled by the almost universal instruction to "take your pulse" after a pacemaker is placed. I think that this may cause more harm than good in the majority of cases.
The problem stems from the fact that your pulse is the expression of the mechanical event of contraction. Your pacemaker does not care about contraction, though - it is an electrical device. There are many circumstances where an electrical event occurs, such as a premature beat, that results in the pacemaker sensing the event and resetting its timers. The premature beat does not result however in sufficient cardiac output for you to register a pulse. If you do the math, the pacemaker will correctly sense all of the beats, and pace at all the right times, yet result in a lower-than-programmed pulse rate.
The manufacturer's instructions suggest that you should take your pulse. Personally, if I had a pacemaker, I wouldn't waste my time or confuse the issue.
©COPY 1997 HeartPoint Updated February 1998
Also see these related topics:
Arrhythmias - Introduction Arrhythmias - General Considerations Arrhythmias - Specific Atrial fibrillation Ventricular arrhythmias
